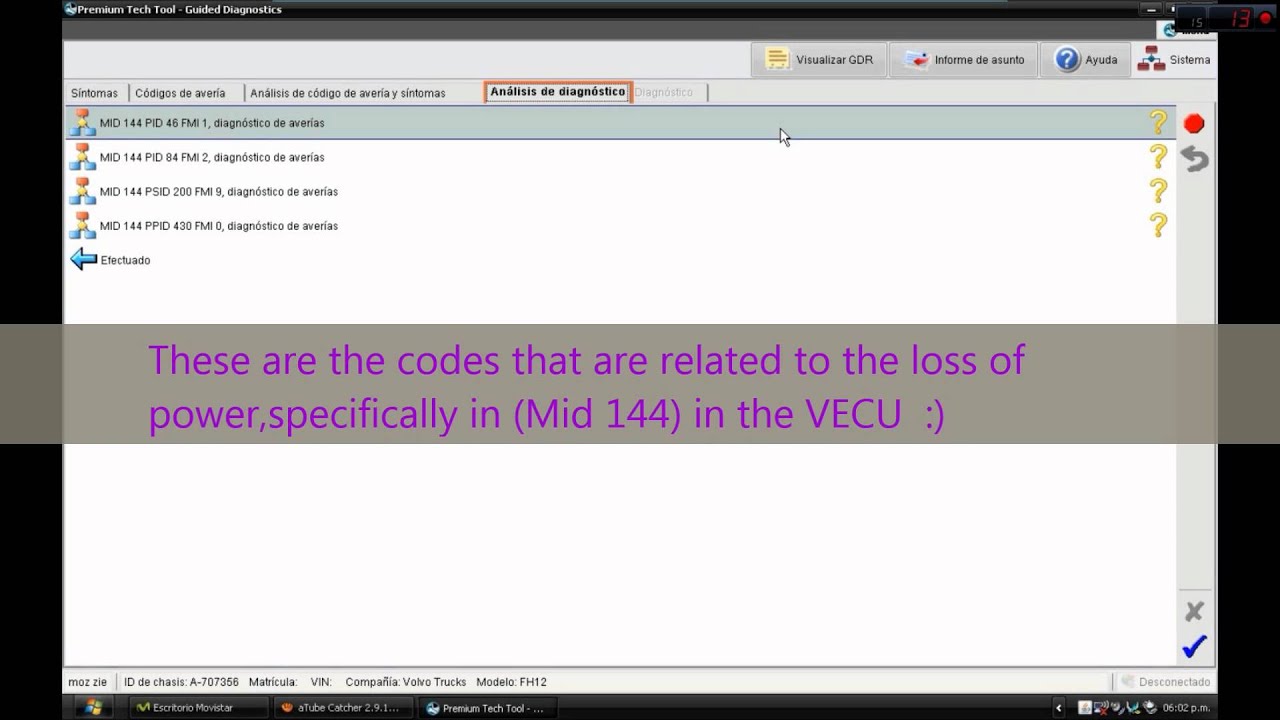
Premium Tech Tool Guided Diagnostics For The Real World

Diagnostic design influence and integration engineering tool. System for the designed diagnostics when deployed to a real-world. DSI INTERNATIONAL. “ We are pleased with our Support.com rollout and are seeing real value from Guided Paths for our agents and interaction. Is The Future of Tech Support.
[] Medical ultrasound (also known as diagnostic sonography or ultrasonography) is a technique based on the application of. It is used to see internal body structures such as,, joints,blood vessels and internal organs. Its aim is often to find a source of a disease or to exclude any. The practice of examining women using ultrasound is called, and is widely used. Is with which are higher than those audible to humans (>20,000 Hz). Ultrasonic images also known as sonograms are made by sending pulses of ultrasound into using a. The sound off the tissue; with different tissues reflecting varying degrees of sound.
These echoes are recorded and displayed as an image to the operator. Many different types of images can be formed using sonographic instruments. The most well-known type is a B-mode image, which displays the acoustic impedance of a two-dimensional cross-section of tissue. Other types of image can display, motion of tissue over time, the location of blood, the presence of specific molecules, the, or the. Compared to other prominent methods of medical imaging, ultrasound has several advantages. It provides images in real-time, it is portable and can be brought to the bedside, it is substantially lower in cost, and it does not use harmful.
Drawbacks of ultrasonography include various limits on its field of view including patient cooperation and physique, difficulty imaging structures behind and air, and its dependence on a skilled operator. Contents • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • By organ or system [ ] Sonography (ultrasonography) is widely used in.
It is possible to perform both and therapeutic procedures, using ultrasound to guide interventional procedures (for instance or drainage of fluid collections). Are medical professionals who perform scans which are then typically interpreted by themselves or the radiologists, physicians who specialize in the application and interpretation of a wide variety of medical imaging modalities, or by cardiologists in the case of cardiac ultrasonography (echocardiography). Sonographers typically use a hand-held probe (called a transducer) that is placed directly on and moved over the patient.
Increasingly, clinicians (physicians and other healthcare professionals who provide direct patient care) are using ultrasound in their office and hospital practices. Sonography is effective for imaging soft tissues of the body.
Superficial structures such as,,,, thyroid and parathyroid glands, and the brain are imaged at a higher (7–18 MHz), which provides better axial and lateral. Deeper structures such as liver and kidney are imaged at a lower frequency 1–6 MHz with lower axial and lateral resolution but greater penetration. A general-purpose ultrasound scanner may be used for most imaging purposes. Usually specialty applications may be served only by use of a specialty transducer. Most ultrasound procedures are done using a transducer on the surface of the body, but improved diagnostic confidence is often possible if a transducer can be placed inside the body. For this purpose, specialty transducers, including endovaginal, endorectal, and transesophageal transducers are commonly employed. At the extreme of this, very small transducers can be mounted on small diameter catheters and placed into blood vessels to image the walls and disease of those vessels.
Anesthesiology [ ] In, Ultrasound is commonly used by anesthesiologists to guide injecting needles when placing local anaesthetic solutions near nerves. It is also used for gaining vascular access such as central venous cannulation and difficult arterial cannulation. Transcranial Doppler is frequently used by neuro-anesthesiologists for obtaining information about flow-velocity in the basal cerebral vessels. Angiology (vascular) [ ].
Further information: and In or vascular medicine, (B Mode vessels imaging combined with Doppler flow measurement) is daily used to diagnose arterial and venous disease all over the body. This is particularly important in, where ultrasound is used for assessing blood flow and stenoses in the carotid arteries () and the big intracerebral arteries (). ( IVUS) is a methodology using a specially designed with a miniaturized probe attached to the distal end of the catheter. The proximal end of the is attached to computerized equipment. It allows the application of technology, such as or, to see from inside out through the surrounding column, visualizing the (inner wall) of in living individuals. Cardiology (heart) [ ].
Further information: and and are frequently used in and. In abdominal sonography, the solid organs of the abdomen such as the,,,,,,, and are imaged. Sound waves are blocked by gas in the bowel and attenuated in different degree by fat, therefore there are limited diagnostic capabilities in this area. The can sometimes be seen when inflamed (as in e.g.: ). Endoanal ultrasound is used particularly in the investigation of anorectal symptoms such as.
It images the immediate perianal anatomy and is able to detect occult defects such as tearing of the anal sphincter. Allows for both detection and characterization. Gynecology and obstetrics [ ]. Main articles: and examines female pelvic organs (specifically the, the, and the ) as well as the, the, and the.
It commonly uses. Is commonly used during to check on the development of the. Otolaryngology (head and neck) [ ] Most structures of the neck, including the and,, and, are well-visualized by high-frequency ultrasound with exceptional anatomic detail. Ultrasound is the preferred imaging modality for thyroid tumors and lesions, and ultrasonography is critical in the evaluation, preoperative planning, and postoperative surveillance of patients with. Many other benign and malignant conditions in the head and neck can be evaluated and managed with the help of diagnostic ultrasound and ultrasound-guided procedures.
Neonatology [ ] In, can be used for basic assessment of intracerebral structural abnormalities, bleeds, or and anoxic insults (). The ultrasound can be performed through the soft spots in the skull of a newborn infant () until these completely close at about 1 year of age and form a virtually impenetrable acoustic barrier for the ultrasound. The most common site for is the anterior fontanelle. The smaller the fontanelle, the poorer the quality of the picture. Ophthalmology ( eyes) [ ] In and, there are two major forms of eye exam using ultrasound: •, commonly referred to as an A-scan (short for Amplitude scan). It is an that provides data on the length of the, which is a major determinant in.
• B-scan ultrasonography, or B-scan, which is a scan that produces a cross-sectional view of the and the. It is commonly used to see inside the eye when media is hazy due to cataract or any corneal opacity. Pulmonology (lungs) [ ] In, endobronchial Ultrasound (EBUS) probes are applied to standard flexible endoscopic probes and used by pulmonologists to allow for direct visualization of endobronchial lesions and lymph nodes prior to transbronchial needle aspiration. Among its many uses, EBUS aids in lung cancer staging by allowing for lymph node sampling without the need for major surgery. Urology (urinary) [ ]. (black butterfly-like shape) and hyperplastic () visualized by medical sonographic technique Ultrasound is routinely used in to determine, for example, the amount of fluid retained in a patient's bladder. In a pelvic sonogram, organs of the pelvic region are imaged.
This includes the and. Males are sometimes given a pelvic sonogram to check on the health of their bladder, the, or their (for example to distinguish from ). In young males, it is used to distinguish more benign testicular masses ( or ) from, which is highly curable but which must be treated to preserve health and fertility. There are two methods of performing a pelvic sonography – externally or internally.
The internal pelvic sonogram is performed either trans (in a woman) or transrectally (in a man). Sonographic imaging of the pelvic floor can produce important diagnostic information regarding the precise relationship of abnormal structures with other pelvic organs and it represents a useful hint to treat patients with symptoms related to pelvic prolapse, double incontinence and obstructed defecation.
It is used to diagnose and, at higher frequencies, to treat (break up) kidney stones or kidney crystals (). Musculoskeletal [ ] ultrasound in used to examine tendons, muscles, nerves, ligaments, soft tissue masses, and bone surfaces. Ultrasound is an alternative to x-ray imaging in detecting fractures of the wrist, elbow and shoulder for patients up to 12 years ().
Quantitative ultrasound is an adjunct musculoskeletal test for myopathic disease in children; estimates of lean body mass in adults; proxy measures of muscle quality (i.e., tissue composition) in older adults with Nephrology (kidneys) [ ]. Main article: In, ultrasonography of the kidneys is essential in the diagnosis and management of kidney-related diseases. The kidneys are easily examined, and most pathological changes in the kidneys are distinguishable with ultrasound. US is an accessible, versatile inexpensive and fast aid for decision-making in patients with renal symptoms and for guidance in renal intervention.
Renal ultrasound (US) is a common examination, which has been performed for decades. Using, assessment of renal anatomy is easily performed, and US is often used as image guidance for renal interventions.
Furthermore, novel applications in renal US have been introduced with contrast-enhanced ultrasound (CEUS), elastography and fusion imaging. However, renal US has certain limitations, and other modalities, such as CT and MRI, should always be considered as supplementary imaging modalities in the assessment of renal disease. From sound to image [ ] The creation of an image from sound is done in three steps – producing a, receiving, and interpreting those echoes. Producing a sound wave [ ]. Medical ultrasound scanner A sound wave is typically produced by a encased in a plastic housing. Strong, short electrical pulses from the ultrasound machine drive the transducer at the desired frequency. The can be anywhere between 1 and 18, though frequencies up to 50–100 megahertz have been used experimentally in a technique known as biomicroscopy in special regions, such as the anterior chamber of the eye.
Older technology transducers focused their beam with physical lenses. Newer technology transducers use techniques to enable the ultrasound machine to change the direction and depth of focus. The sound is focused either by the shape of the transducer, a lens in front of the transducer, or a complex set of control pulses from the ultrasound scanner, in the () technique. This focusing produces an arc-shaped sound wave from the face of the transducer. The wave travels into the body and comes into focus at a desired depth. Builddesk U Keygen For Mac.
Materials on the face of the transducer enable the sound to be transmitted efficiently into the body (often a rubbery coating, a form of ). In addition, a water-based gel is placed between the patient's skin and the probe. The sound wave is partially reflected from the layers between different tissues or scattered from smaller structures. Specifically, sound is reflected anywhere where there are acoustic impedance changes in the body: e.g. In, small structures in organs, etc.
Some of the reflections return to the transducer. Receiving the echoes [ ] The return of the sound wave to the transducer results in the same process as sending the sound wave, except in reverse. The returned sound wave vibrates the transducer and the transducer turns the vibrations into electrical pulses that travel to the ultrasonic scanner where they are processed and transformed into a digital image. Forming the image [ ] To make an image, the ultrasound scanner must determine two things from each received echo: • How long it took the echo to be received from when the sound was transmitted. • How strong the echo was. Once the ultrasonic scanner determines these two things, it can locate which pixel in the image to light up and to what intensity. Transforming the received signal into a digital image may be explained by using a blank spreadsheet as an analogy.
First picture a long, flat transducer at the top of the sheet. Send pulses down the 'columns' of the spreadsheet (A, B, C, etc.).
Listen at each column for any return echoes. When an echo is heard, note how long it took for the echo to return. The longer the wait, the deeper the row (1,2,3, etc.). The strength of the echo determines the brightness setting for that cell (white for a strong echo, black for a weak echo, and varying shades of grey for everything in between.) When all the echoes are recorded on the sheet, we have a greyscale image. Displaying the image [ ] Images from the ultrasound scanner are transferred and displayed using the standard. Normally, very little post processing is applied to ultrasound images.
Sound in the body [ ]. B-flow image of. • B-flow is a mode that digitally highlights weak flow reflectors (mainly ) while suppressing the signals from the surrounding stationary tissue. It can visualize flowing blood and surrounding stationary tissues simultaneously.
• C-mode: A C-mode image is formed in a plane normal to a B-mode image. A gate that selects data from a specific depth from an A-mode line is used; then the transducer is moved in the 2D plane to sample the entire region at this fixed depth.
When the transducer traverses the area in a spiral, an area of 100 cm 2 can be scanned in around 10 seconds. • M-mode: In M-mode (motion mode) ultrasound, pulses are emitted in quick succession – each time, either an A-mode or B-mode image is taken. Over time, this is analogous to recording a in ultrasound. As the organ boundaries that produce reflections move relative to the probe, this can be used to determine the velocity of specific organ structures. Duplex scan of the common carotid artery is employs the to assess whether structures (usually blood) are moving towards or away from the probe, and its relative velocity. By calculating the frequency shift of a particular sample volume, for example flow in an artery or a jet of blood flow over a heart valve, its speed and direction can be determined and visualized. Color Doppler is the measurement of velocity by color scale.
Color Doppler images are generally combined with grayscale () images to display duplex ultrasonography images. Uses include: •, the use of Doppler ultrasonography to examine the.
An echocardiogram can, within certain limits, produce accurate assessment of the direction of and the of blood and cardiac tissue at any arbitrary point using the Doppler effect. Velocity measurements allow assessment of areas and function, any abnormal communications between the left and right side of the heart, any leaking of blood through the valves (), calculation of the and calculation of (a measure of ). Contrast-enhanced ultrasound using gas-filled microbubble contrast media can be used to improve velocity or other flow-related medical measurements. • (TCD) and transcranial color Doppler (TCCD), which measure the velocity of through the 's transcranially (through the ).
They are used as to help diagnose,, from a subarachnoid (bleeding from a ruptured ), and other problems. •, although usually not technically but rather sound-generating, use the Doppler effect to detect the for. These are hand-held, and some models also display the in beats per minute (BPM). Use of this monitor is sometimes known as Doppler. The Doppler fetal monitor is commonly referred to simply as a Doppler or fetal Doppler. Doppler fetal monitors provide information about the fetus similar to that provided by a.
Contrast ultrasonography (ultrasound contrast imaging) [ ]. Main article: A for medical ultrasonography is a formulation of encapsulated gaseous microbubbles to increase of blood, discovered by Dr Raymond Gramiak in 1968 and named. This contrast modality is clinically used throughout the world, in particular for in the United States and for in and. Microbubbles-based contrast media is administrated in during the medical ultrasonography examination. The microbubbles being too large in diameter, they stay confined in and cannot extravasate towards the. An contrast media is therefore purely intravascular, making it an ideal agent to image microvascularization for purposes. A typical clinical use of contrast ultrasonography is detection of a, which exhibits a contrast uptake (kinetics of microbubbles concentration in blood circulation) faster than healthy surrounding the tumor.
Other clinical applications using contrast exist, such as in to improve delineation of for visually checking contractibility of after a. Finally, applications in quantitative perfusion (relative measurement of ) emerge for identifying early patient response to an anti-cancerous drug treatment (methodology and clinical study by Dr Nathalie Lassau in 2011 ), enabling to determine the best therapeutic options.
Parametric imaging of vascular signatures (diagram) In oncological practice of medical contrast ultrasonography, clinicians use the method of parametric imaging of vascular signatures invented by Dr Nicolas Rognin in 2010. This method is conceived as a aided diagnostic tool, facilitating characterization of a suspicious ( versus ) in an organ. This method is based on medical to analyze a time sequence of ultrasound contrast images, a digital video recorded in real-time during patient examination. Two consecutive steps are applied to each of the tumor: • calculation of a vascular signature (contrast uptake difference with respect to healthy tissue surrounding the tumor); • automatic of the vascular signature into a unique, this last coded in one of the four following: • for continuous hyper-enhancement (contrast uptake higher than healthy tissue one), • for continuous hypo-enhancement (contrast uptake lower than healthy tissue one), • for fast hyper-enhancement (contrast uptake before healthy tissue one) or • for fast hypo-enhancement (contrast uptake after healthy tissue one). Once in each pixel completed, a color spatial map of the parameter is displayed on a, summarizing all information of the tumor in a single image called parametric image (see last figure of press article as clinical examples). This parametric image is interpreted by clinicians based on predominant colorization of the tumor: red indicates a suspicion of (risk of cancer), green or yellow – a high probability of. In the first case (suspicion of ), the clinician typically prescribes a biopsy to confirm the diagnostic or a examination as a second opinion.
In the second case (quasi-certain of ), only a follow-up is needed with a contrast ultrasonography examination a few months later. The main clinical benefits are to avoid a systematic biopsy (risky invasive procedure) of benign tumors or a examination exposing the patient to radiation. The parametric imaging of vascular signatures method proved to be effective in humans for characterization of tumors in the liver. In a context, this method might be potentially applicable to other organs such as. Molecular ultrasonography (ultrasound molecular imaging) [ ] The future of contrast ultrasonography is in with potential clinical applications expected in to detect at their earliest stage of appearance.
Molecular ultrasonography (or ultrasound molecular imaging) uses targeted microbubbles originally designed by Dr in 1997; such targeted microbubbles specifically bind or adhere to tumoral microvessels by targeting cancer expression (overexpression of certain biomolecules occurs during or processes in malignant tumors). As a result, a few minutes after their injection in blood circulation, the targeted microbubbles accumulate in the malignant tumor; facilitating its localization in a unique ultrasound contrast image. In 2013, the very first exploratory in humans for was completed at in the by Dr Hessel Wijkstra. In molecular ultrasonography, the technique of (also used for shear wave ) is applied in order to literally push the targeted microbubbles towards microvessels wall; firstly demonstrated by Dr Paul Dayton in 1999.
This allows to maximize binding to the malignant tumor; the targeted microbubbles being in more direct contact with cancerous biomolecules expressed at the inner surface of tumoral microvessels. At the stage of scientific research, the technique of acoustic radiation force was implemented as a prototype in clinical ultrasound systems and validated in 2D and 3D imaging modes. Elastography (ultrasound elasticity imaging) [ ]. Main article: Ultrasound is also used for elastography, which is a relatively new imaging modality that maps the elastic properties of soft tissue. This modality emerged in the last two decades. Elastography is useful in medical diagnoses as it can discern healthy from unhealthy tissue for specific organs/growths. For example, cancerous tumors will often be harder than the surrounding tissue, and diseased livers are stiffer than healthy ones.
There are many ultrasound elastography techniques. The most prominent are: Quasistatic Elastography/Strain Imaging, Shear Wave Elasticity Imaging (SWEI), Supersonic Shear Imaging (SSI), Acoustic Radiation Force Impulse imaging (ARFI), and Transient Elastography. The steadily growing clinical use of ultrasound elastography is a result of the implementation of technology in clinical ultrasound machines. Currently, an increase of activities in the field of elastography is observed demonstrating successful application of the technology in various areas of medical diagnostics and treatment monitoring.
Interventional ultrasonography [ ] Interventional ultrasonography involves, emptying fluids, intrauterine (). •: The high frequency thyroid (HFUS) can be used to treat several gland conditions. The recurrent thyroid cyst that was usually treated in the past with surgery, can be treated effectively by a new procedure called percutaneous ethanol injection, or PEI. With ultrasound guided placement of a 25 gauge needle within the cyst, and after evacuation of the cyst fluid, about 50% of the cyst volume is injected back into the cavity, under strict operator visualization of the needle tip. The procedure is 80% successful in reducing the cyst to minute size. • Metastatic thyroid cancer neck lymph nodes: The other thyroid therapy use for HFUS is to treat metastatic thyroid cancer neck lymph nodes that occur in patients who either refuse surgery, or are no longer a candidate for surgery. Small amounts of ethanol are injected under ultrasound guided needle placement.
A blood flow study is done prior to the injection, by power doppler. The blood flow can be destroyed and the node become inactive, although it may still be there. Power doppler visualized blood flow can be eradicated, and there may be a drop in the cancer blood marker test,, TG, as the node become non-functional. Another interventional use for HFUS is to mark a cancer node one hour prior to surgery to help locate the node cluster at the surgery. A minute amount of methylene dye is injected, under careful ultrasound guided placement of the needle on the anterior surface, but not in the node. The dye will be evident to the thyroid surgeon when he opens the neck.
A similar localization procedure with methylene blue, can be done to locate parathyroid adenomas at surgery. Compression ultrasonography [ ] Compression ultrasonography is a simplified technique used for quick diagnosis. The examination is limited to and only, instead to spend time performing the full examination,. It is performed using only one test: vein compression.
Compression ultrasonography has both high for detecting proximal deep vein thrombosis only in symptomatic patients. Results are not reliable when the patient is symptomless and must be checked, for example in high risk postoperative patients mainly in orthopedic patients. Attributes [ ] As with all imaging modalities, ultrasonography has its list of positive and negative attributes.
Strengths [ ] • It images,, and bone surfaces very well and is particularly useful for delineating the interfaces between solid and fluid-filled spaces. • It renders 'live' images, where the operator can dynamically select the most useful section for diagnosing and documenting changes, often enabling rapid diagnoses. Live images also allow for ultrasound-guided biopsies or injections, which can be cumbersome with other imaging modalities.
• It shows the structure of organs. • It has no known long-term side effects and rarely causes any discomfort to the patient. • Equipment is widely available and comparatively flexible.
• Small, easily carried scanners are available; examinations can be performed at the bedside. • Relatively inexpensive compared to other modes of investigation, such as,. • is better in high frequency ultrasound transducers than it is in most other imaging modalities. • Through the use of an, an ultrasound device can offer a relatively inexpensive, real-time, and flexible method for capturing data required for special research purposes for tissue characterization and development of new image processing techniques Weaknesses [ ].
Double aort artifact in sonography due to difference in velocity of sound waves in muscle and fat. • Sonographic devices have trouble penetrating. For example, sonography of the adult brain is currently very limited. • Sonography performs very poorly when there is a gas between the transducer and the organ of interest, due to the extreme differences in. For example, overlying gas in the gastrointestinal tract often makes ultrasound scanning of the difficult.
Lung imaging however can be useful in demarcating pleural effusions, detecting, and detecting pneumonia. • Even in the absence of bone or air, the depth penetration of ultrasound may be limited depending on the frequency of imaging. Consequently, there might be difficulties imaging structures deep in the body, especially in obese patients. • Physique has a large influence on image quality.
Image quality and accuracy of diagnosis is limited with obese patients, overlying subcutaneous fat attenuates the sound beam and a lower frequency transducer is required (with lower resolution) • The method is operator-dependent. A high level of skill and experience is needed to acquire good-quality images and make accurate diagnoses. • There is no scout image as there is with CT and MRI. Once an image has been acquired there is no exact way to tell which part of the body was imaged.
Risks and side-effects [ ] Ultrasonography is generally considered safe imaging, with the World Health Organizations saying: 'Diagnostic ultrasound is recognized as a safe, effective, and highly flexible imaging modality capable of providing clinically relevant information about most parts of the body in a rapid and cost-effective fashion'. Diagnostic ultrasound studies of the fetus are generally considered to be safe during pregnancy. This diagnostic procedure should be performed only when there is a valid medical indication, and the lowest possible ultrasonic exposure setting should be used to gain the necessary diagnostic information under the 'as low as reasonably practicable' or principle. However, medical ultrasonography should not be performed without a medical indication to perform it. To do otherwise would be to perform to patients, which bring unwarranted costs and may lead to other testing. Overuse of ultrasonography is sometimes, especially as routine screening for deep vein thrombosis after orthopedic surgeries in patients who are not at heightened risk for having that condition. Similarly, although there is no evidence ultrasound could be harmful for the fetus, medical authorities typically strongly discourage the promotion, selling, or leasing of ultrasound equipment for making 'keepsake fetal videos'.
Studies on the safety of ultrasound [ ] • A meta-analysis of several ultrasonography studies published in 2000 found no statistically significant harmful effects from ultrasonography, but mentioned that there was a lack of data on long-term substantive outcomes such as neurodevelopment. • A study at the published in 2006 found a small but significant correlation between prolonged and frequent use of ultrasound and abnormal neuronal migration in mice. • A study performed in Sweden in 2001 has shown that subtle effects of neurological damage linked to ultrasound were implicated by an increased incidence in left-handedness in boys (a marker for brain problems when not hereditary) and speech delays. • The above findings, however, were not confirmed in a later follow-up study. • A later study, however, performed on a larger sample of 8865 children, has established a statistically significant, albeit weak association of ultrasonography exposure and being non-right handed later in life. Obstetric ultrasound [ ].
Main article: Obstetric ultrasound can be used to identify many conditions that would be harmful to the mother and the baby, many health care professionals consider the risk of leaving these conditions undiagnosed to be much greater than the very small risk, if any, associated with undergoing an ultrasound scan. However its results are occasionally incorrect, producing a false positive (the is a relevant effort to improve the reliability of health care trials). False detection may result in patients being warned of birth defects when no such defect exists. When balancing risk and reward, there are recommendations to avoid the use of routine ultrasound for low risk pregnancies; [ ] but in many countries ultrasound is now used routinely in the management of all pregnancies. [ ] Sex determination is only accurate after 12 weeks gestation. Even where is used routinely in obstetric appointments during pregnancy, authorities discourage its use for non-medical purposes such as fetal 'keepsake' videos and photos.
Obstetric ultrasound is primarily used to: • Date the pregnancy () • Confirm fetal viability • Determine location of, intrauterine vs • Check the location of the placenta in relation to the cervix • Check for the number of fetuses () • Check for major physical abnormalities. • Assess fetal growth (for evidence of ()) • Check for fetal movement and heartbeat. • Determine the sex of the baby According to the European Committee of Medical Ultrasound Safety (ECMUS) Ultrasonic examinations should only be performed by competent personnel who are trained and updated in safety matters. Ultrasound produces heating, pressure changes and mechanical disturbances in tissue. Diagnostic levels of ultrasound can produce temperature rises that are hazardous to sensitive organs and the embryo/fetus.
Biological effects of non-thermal origin have been reported in animals but, to date, no such effects have been demonstrated in humans, except when a microbubble is present. Nonetheless, care should be taken to use low power settings and avoid pulsed wave scanning of the fetal brain unless specifically indicated in high risk pregnancies. Ultrasound scanners have different -techniques to visualize arteries and veins. The most common is colour doppler or power doppler, but also other techniques like b-flow are used to show bloodflow in an organ. By using pulsed wave doppler or continuous wave doppler bloodflow velocities can be calculated. Figures released for the period 2005–2006 by the UK Government (Department of Health) show that non-obstetric ultrasound examinations constituted more than 65% of the total number of ultrasound scans conducted.
Society and culture [ ] Recent studies have stressed the importance of framing “reproductive health matters cross-culturally”, particularly when understanding the “new phenomenon” of “the proliferation of ultrasound imaging” in developing countries. In 2004, Tine Gammeltoft interviewed 400 women in Hanoi’s Obstetrics and Gynecology Hospital; each “had an average of 6.6 scans during her pregnancy”, much higher than five years ago when “a pregnant woman might or might not have had a single scan during her pregnancy” in Vietnam. Gammeltoft explains that “many Asian countries” see “the foetus as an ambiguous being” unlike in Western medicine where it is common to think of the foetus as “materially stable”. Therefore, although women, particularly in Asian countries, “express intense uncertainties regarding the safety and credibility of this technology”, it is overused for its “immediate reassurance”. Regulation [ ] Diagnostic and therapeutic ultrasound equipment is regulated in the USA by the, and worldwide by other national regulatory agencies. The FDA limits acoustic output using several metrics; generally, other agencies accept the FDA-established guidelines.
Currently, New Mexico, Oregon, and North Dakota are the only US states that regulate diagnostic medical sonographers. Certification examinations for sonographers are available in the US from three organizations: the, and the.
[ ] The primary regulated metrics are (MI), a metric associated with the cavitation bio-effect, and Thermal Index (TI) a metric associated with the tissue heating bio-effect. Download Ufc Keygen there. The FDA requires that the machine not exceed established limits, which are reasonably conservative so as to maintain diagnostic ultrasound as a safe imaging modality. This requires on the part of the manufacturer in terms of the machine's calibration. Ultrasound-based pre-natal care and sex screening technologies were launched in India in the 1980s. With concerns about its misuse for, the Government of India passed the in 1994 to regulate legal and illegal uses of ultrasound equipment.
The law was further amended into the Pre-Conception and Pre-natal Diagnostic Techniques (Regulation and Prevention of Misuse) (PCPNDT) Act in 2004 to deter and punish prenatal sex screening and sex selective abortion. It is currently illegal and a punishable crime in India to determine or disclose the sex of a fetus using ultrasound equipment. History [ ] After the French physicist ’s discovery of in 1880, ultrasonic waves could be deliberately generated for industry. Thereafter, in 1940, the American acoustical physicist devised the first ultrasonic echo imaging device, the Supersonic Reflectoscope, to detect internal flaws in metal castings.
In 1941, the Austrian neurologist Karl Theo Dussik was in collaboration with his brother, Friedreich, a physicist, likely, the first person to ultrasonically echo image the human body, outlining thereby the ventricles of a human brain. Ultrasonic energy was first applied to the human body for medical purposes by Dr at the Naval Medical Research Institute, in the late 1940s. English-born physicist (1914–2009) first used ultrasound to assess the thickness of bowel tissue as early as 1949; he has been described as the 'father of medical ultrasound'. Subsequent advances in the field took place concurrently in several countries. France [ ] In his book 'L'investigation vasculaire par ultrasonographie Doppler' (Ed Masson, 1977) Dr laid down the Doppler Ultrasound fundamentals of the hemodynamics semiotics, which are still in use in current Doppler arterial and venous Duplex Ultrasound investigations. Scotland [ ] Parallel developments in, Scotland by Professor and colleagues at the (GRMH) led to the first diagnostic applications of the technique. Donald was an with a self-confessed 'childish interest in machines, electronic and otherwise', who, having treated the wife of one of the company's directors, was invited to visit the Research Department of boilermakers at, where he used their industrial ultrasound equipment to conduct experiments on various morbid anatomical specimens and assess their ultrasonic characteristics.
Together with the medical physicist (; ). And fellow obstetrician Dr John MacVicar, Donald refined the equipment to enable differentiation of pathology in live volunteer patients. These findings were reported in on 7 June 1958 as 'Investigation of Abdominal Masses by Pulsed Ultrasound' – possibly one of the most important papers ever published in the field of diagnostic. At GRMH, Professor Donald and Dr James Willocks then refined their techniques to obstetric applications including fetal head measurement to assess the size and growth of the fetus. With the opening of the new Queen Mother's Hospital in in 1964, it became possible to improve these methods even further. Dr 's pioneering work on led to it acquiring long-term status as the definitive method of study of foetal growth. As the technical quality of the scans was further developed, it soon became possible to study pregnancy from start to finish and diagnose its many complications such as multiple pregnancy, fetal abnormality and.
Diagnostic ultrasound has since been imported into practically every other area of medicine. Sweden [ ] Medical ultrasonography was used in 1953 at by and 's son, who was then a graduate student at the University's department of. Edler had asked Hertz if it was possible to use to look into the body, but Hertz said this was impossible. However, he said, it might be possible to use ultrasonography.
Hertz was familiar with using ultrasonic reflectoscopes of the American acoustical physicist 's invention for, and together Edler and Hertz developed the idea of using this method in medicine. The first successful measurement of heart activity was made on October 29, 1953 using a device borrowed from the ship construction company in. On December 16 the same year, the method was used to generate an echo-encephalogram (ultrasonic probe of the ). Edler and Hertz published their findings in 1954. United States [ ] In 1962, after about two years of work, Joseph Holmes, William Wright, and Ralph Meyerdirk developed the first compound contact B-mode scanner.
Their work had been supported by and the. Wright and Meyerdirk left the University to form Physionic Engineering Inc., which launched the first commercial hand-held articulated arm compound contact B-mode scanner in 1963. This was the start of the most popular design in the history of ultrasound scanners. In the late 1960s and the bio-engineering group at the conducted research on Doppler ultrasound as a diagnostic tool for vascular disease. Eventually, they developed technologies to use duplex imaging, or Doppler in conjunction with B-mode scanning, to view vascular structures in real-time, while also providing hemodynamic information. The first demonstration of color Doppler was by Geoff Stevenson, who was involved in the early developments and medical use of Doppler shifted ultrasonic energy. See also [ ] • • • • • • References [ ].